A New Framework Prioritizes Continuous Improvement During PCRA

For more than two decades, The Centers for Medicare and Medicaid Services (CMS) and The Joint Commission (TJC) has required U.S. hospitals to assess and reduce risks from construction, renovation, and maintenance projects. While TJC’s Pre-Construction Risk Assessment (PCRA) standard lays out the requirements, it does not offer a roadmap for compliance – or for carrying out a program focused on continuous monitoring and performance improvement.
Or does it? It turns out that through a framework, developed by EH&E and one of our clients, that extends the pre-construction risk assessment process from the design concept all the way through post-construction closeout, project managers can ensure risk-reduction practices are followed from design through occupancy.
What is PCRA?
The pre-construction risk assessment is essential for identifying and mitigating all of the potential risks associated with construction debris, noise, and potentially hazardous processes or materials. TJC’s PCRA standard is meant to be carried through the entire construction process and for a broad set of risks to patients and staff, but this is not always effectively done. Yet with a more holistic view of PCRA, and application of a simple framework, project managers can drive improvements throughout the construction process.
How to enhance PCRA
As with any project, this framework is most impactful when it follows four consistent steps: initiate, plan, execute, and closeout. Each element enhances conventional practices, and we’ve seen the powerful impact of this approach in action. During construction at one of the nation’s top 10 children’s hospitals, this framework led to a threefold decrease in the number of high-risk issues noted on construction site audits during construction.
Hospitals ready to standardize PCRA throughout the entire construction process – from design review through handover – can begin by implementing best practices outlined in the four phases below.
Phase 1: Initiate
Most hospitals begin the PCRA process during the construction planning phases, typically a few weeks to a few months before construction containment goes up. However, there are significant benefits to bringing stakeholders from safety, facilities, clinical engineering, and infection control, as well as end users, into the project earlier during the design review phase – as early as several months to more than a year before construction containment goes up. This early involvement provides an opportunity to identify potential conflicts and noncompliance issues while it is easier and more cost-effective to make changes.
We recommend securing feedback from the integrated team at two critical junctures: the 30% and 75% design review phases. At 30% of the design review, there is a preliminary sketch ready for any sweeping changes or considerations. When the design is at 75%, stakeholders can begin to offer more nuanced feedback.
Engaging this diverse set of stakeholders early can also help secure buy-in as hospitals prepare to update their pre-construction risk assessment process, including potentially using ASHE’s ICRA 2.0. The PCRA process can be challenging, but early input allows stakeholders to identify areas of frustration and then work together to align goals, facilitate cross-functional collaboration, and streamline the entire process.
Phase II: Plan
This phase makes up the core of most hospitals’ current PCRA programs and is the area that organizations tend to be most familiar with and prepared to manage. The planning phase is the time to standardize PCRA processes to ensure all high-risk issues are addressed and that teams understand their roles and what to expect at each meeting. Conducting reviews and establishing outputs for safety, infection control, and logistics make it easier to chart success. Detailed meeting checklists also help establish consistency.
This is also the time to begin drafting and implementing isolation practices – a difficult practice, due to the complex nature of mechanical systems and the variety of patient areas. Collaboration between infection control and facilities teams can help project managers better match potential risks to appropriate containment measures by drawing upon a broader range of knowledge.
Implementing isolation practices requires standardization, as has been proposed in ASHE ICRA 2.0, However, one-size-fits-all approaches may not fit for the most complex hospital projects. Complex scenarios (e.g., construction involving multiple floors, removal of the façade, etc.) warrant professional engineering and industrial hygiene review, or at least highly specialized expertise, to protect patients from harm.
Phase III: Execute
During construction, weekly site audits that use checklists to find and document issues can provide valuable data that can guide improvements. Audits should be led by multidisciplinary teams.
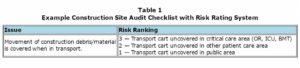
By rating the risks that inspection items identify during these audits, it becomes possible to prioritize action. While all violations are important to address, some issues that can cause direct harm require a more immediate response than others. Ranking these issues empowers project managers to quickly resolve high-risk issues without losing sight of other violations that need to be addressed.
To rank risk, assign inspection items in the construction safety audit a risk rating from 1 to 3, with 3 being the most serious violation (see Table 1). Follow-up actions can then be prioritized based upon the level of risk identified.
When this ranking is coupled with a “report card” process for evaluating contractors, project teams can enhance contractor accountability. A report card is simply a process by which project managers can track issues for greater visibility into trends over time. With this data in hand, project managers can deliver to their contractor partners insight into violations that may need to be addressed through training or changes to their internal practices. This also benefits contractors by showing how they will be evaluated and demonstrating that all contractors will be evaluated on the same basis.
Phase IV: Close-out
While PCRA is intended to reduce risk throughout the entire construction process, it is not always effectively utilized during the construction closeout/pre-occupancy phase. Using a pre-occupancy checklist that requires key stakeholders’ approvals can ensure the environment is ready for occupancy in full compliance with organizational and regulatory or accreditation requirements. This process can also reduce move-in delays caused by minor oversights such as missing medical equipment inspection stickers, construction dust on furniture, or punch list issues that can impact staff or patient comfort and safety.
Continue driving improvement
Standardization, design reviews, and risk-based inspection metrics that create accountability and better “close-out” preoccupancy processes can breathe new value into the pre-construction risk assessment process. By driving performance improvement, this framework moves PCRA beyond compliance and helps hospitals trust that they are effectively mitigating potential risks to patients and staff.
Hospitals that have adopted this framework have found additional value in converting these PCRA metrics to key performance indicators they could present to hospital leadership and use within the hospital’s annual Environment of Care report. This built greater value upon their success and ensured future vulnerabilities were identified quickly.
Want to apply this enhanced PCRA framework to your next project? Reach out to the professionals at EH&E any time with questions or to discuss opportunities to partner on a safe, effective PCRA process.
Subscribe
to our blog
"*" indicates required fields