Nonpharmaceutical Interventions Work: What Every Industry Can Learn from Summer Camps

The arrival of vaccines to help control the COVID-19 pandemic is encouraging, but the truth is that a proven effective medical intervention will still take time to distribute and administer and for immunity to develop. And while physicians and researchers are making progress in treatment and medicines for COVID-19, it remains a reactive approach. Fortunately, there is ample evidence that nonpharmaceutical interventions (NPIs) work.
Nonpharmaceutical interventions are strategies layered upon one another in order to avoid the introduction of potentially infected people into a particular situation and to limit the spread of SARS-CoV-2 within a group. What’s more, we know this layered approach to protection works, based on extensive evidence in day and overnight camp settings from spring and summer 2020 as well as schools with in-person and hybrid operations. Through a research study with the American Camp Association (ACA), we’ve provided evidence that the NPI strategy can avoid introduction of infected individuals into camp and limit secondary transmission of SARS-CoV-2 when all stakeholders adhere to recommended best practices.
Layering protection with nonpharmaceutical interventions
There are a number of nonpharmaceutical interventions that can be applied to limit the transmission of viruses in our organizations, our communities, our states, our countries, and globally. Each layer offers some level of protection, but also carries its own challenges.
- PPE: While PPE (personal protective equipment), such as N95 respirators, reliably protects the wearer and people around them, we’ve seen clear evidence of its limitations: availability. Due to limited supplies, this solution is best reserved for individuals most at risk of exposure (i.e., frontline workers), giving it limited effectiveness in reducing transmission on its own.
- Administrative controls: Commercial office buildings, schools, camps and others are reducing occupancy and interactions through use of small group cohorts. This cohort strategy ensures that if an infection enters the workplace, classroom or camp, secondary transmission of that infection is confined to the small group. This allows individuals to isolate themselves in quarantine without shutting down the broader operation. Administrative controls such as physical distancing are key to limiting the spread of an infection once it has entered into a particular population.
- Physical and engineering controls: By making changes to the environment, people have been able to safely return to many pre-pandemic pursuits. These controls include face mask wearing, increased ventilation in buildings, and surface disinfection.
- Substitution: Moving indoor activities outdoors and replacing high-contact activities with low-contact activities are all practical examples of substitution. Some camps, for example, have moved to replacing basketball games with basketball drills that limit campers’ exposure to one another’s respiratory droplets.
- Elimination: We’ve seen the efficacy of this approach of eliminating contact between people through lockdowns of schools, businesses and nations. However, this most successful nonpharmaceutical intervention category is also the most disruptive.
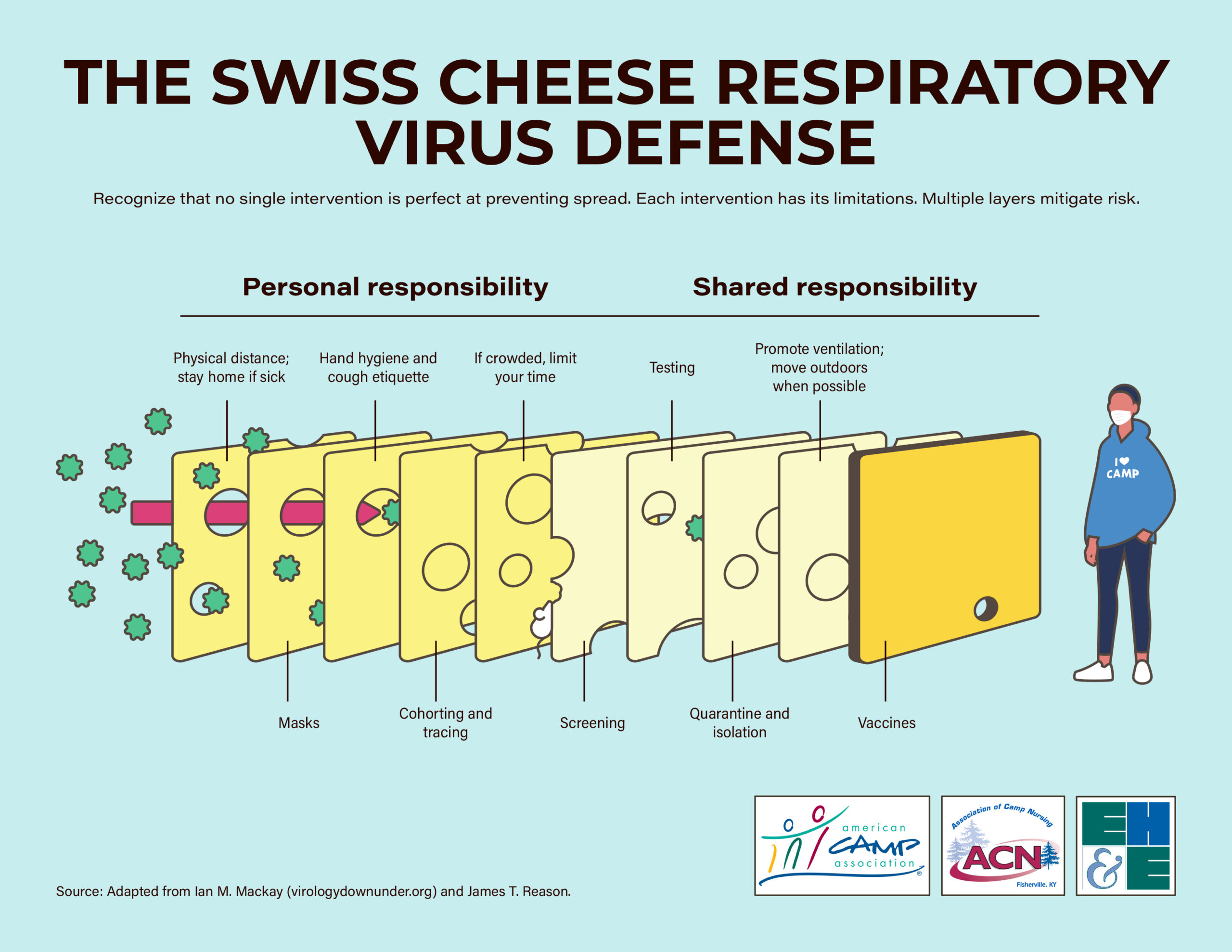
It’s important to note that the greatest value of these nonpharmaceutical interventions comes in a layered approach. Epidemiologists are increasingly referring to this as the “Swiss cheese” defense, based on the “Swiss Cheese Model” James Reason introduced in 1990 to address workplace risks. The thinking goes that each layer of protection has some weaknesses or “holes.” People may forget to wear their masks or not wash their hands as often as they should. They may cough into their hands instead of into their sleeve or forget to avoid touching their face. However, by relying on a range of strategies, there is another “layer” or safeguard available to stop viral transmission should one strategy be circumvented.
Building on this defense, the collective efforts by leadership to implement measures to address infection risks such as testing and ventilation can be viewed as adding layers of protection. The introduction of vaccines is like adding a second layer of thick Cheddar Cheese that backs the NPI strategy for greater effectiveness. Transitioning the defense strategy to what is now being called the “Swiss and Cheddar Cheese Defense Model”.
What camp has taught us about the effectiveness of nonpharmaceutical interventions
Through research, such as the ACA study and published papers in the US and around the world on child congregate settings and SARS-CoV-2 transmission, we now have evidence that this reliance on nonpharmaceutical interventions works. Several recent studies of overnight camps provide an interesting look at the benefit of layering these interventions. Camps also provide a particularly unique perspective in that they offer insight into a cross-section of adult and youth populations, giving lessons learned here applicability in a range of other settings, including daycare, K-12 schools, and higher education institutions, as well as offices, gymnasiums, hair salons, and airplanes.
Among these studies is an examination of how a multi-layered approach to nonpharmaceutical interventions helped four overnight Maine camps reduce the level of infections coming into the camp and ultimately eliminate secondary transmissions. In this case, more than 1,000 camp attendees, from 7-year-old campers to 70-year-old staff, were asked to quarantine with their family for at least 10 days before arriving at camp and test for SARS-CoV-2 in the week leading up to camp. Nonpharmaceutical interventions implemented at camp included small group cohorting, daily screening for fever and COVID-19 symptoms, mask requirements, and substitution of indoor activities for outside sports that allowed for social distancing.
Three asymptomatic attendees at three different camps received positive SARS-CoV-2 test results after arrival at camp and were rapidly isolated and their cohorts were quarantined for 14 days per state and CDC guidance. No secondary transmission was identified.
A similar study of more than 22 overnight camps in Barcelona also found a strategy that focused on layering nonpharmaceutical interventions to be effective in limiting infections coming in and preventing secondary transmission. A five-week research study from the SJD Barcelona Children’s Hospital identified 39 cases of coronavirus in what researchers called a school-like environment. Campers and staff used layers of nonpharmaceutical interventions including frequent hand washing, small group cohorting, mask-wearing, and primarily outdoor activities. From those pediatric cases, researchers identified a 4.6% rate of secondary infection, a number they called six times lower than that of the general population at the time of study.
On the other hand, there is also evidence emerging as to the results of relaxing use of nonpharmaceutical interventions. In June, a Georgia overnight camp was forced to close after an outbreak. An investigation indicated that staff members were allowed to remove masks and there was no requirement to increase ventilation by opening windows and doors. Of the 344 campers tested, 260 tests ultimately came back positive.
Similarly, a Wisconsin camp saw 118 campers (76% of attendees) test positive for SARS-CoV-2, which investigators indicated likely resulted from a single student who had tested negative on a RT-PCR test less than a week before arriving at camp. The camp had required documentation of a negative RT-PCR test prior to arrival, a 7-day prearrival quarantine, and outdoor programming, but did not implement other recommended nonpharmaceutical interventions. CDC investigators concluded that, due to the size of the camp, retreat organizers quickly lost the ability to contain transmission through isolation and quarantine measures.
Encourage a proactive approach
These findings provide not only evidence that nonpharmaceutical interventions work, but also reasonable direction on how to apply these interventions in a variety of settings. A layered approach that accounts for a range of control levels—including PPE, administrative controls, substitution and, in the case of positive tests, elimination—is truly necessary to lower transmission levels and contain spread to prevent outbreaks of SARS-CoV-2.
While testing will remain a necessity to confirm that the layers work and that individuals are adhering to recommended practices, that remains a reactive approach to the problem. To lower transmission rates and proactively keep one another safe at school, at work and at camp, a layered NPI approach is proven to work.
If you’re not sure which layers may prove most effective in keeping your environment safe, EH&E can help. Contact our team of public and environmental health and safety professionals, and engineers to learn how they can apply their expertise to help your organization create an effective path forward.
Subscribe
to our blog
"*" indicates required fields